Body Acne Is Present in about 50% of People Who Have Facial Acne

The Essential Info
While it may sound surprising because people are usually covered up, body acne is present in about 50% of people who have facial acne.
Body acne that is not accompanied by facial acne occurs in only a small proportion of people.
My Experience: Body acne always came along with facial acne for me. In fact, my body acne was worse than my facial acne in college. Even as an adult, body acne stuck around, albeit to a lesser degree than facial acne stuck around. One thing I noticed–and this is anecdotal because I am just one person–is that my body acne responded very well to eating a low-carb, keto-type diet. While I was not able to completely clear my facial acne with eating low-carb, my body acne faded away pretty quickly so long as I stayed low-carb.

The Science
- About One-Half of People with Facial Acne Also Suffer from Body Acne
- Body Acne Often Goes Unreported
- Not Enough Research on Body Acne
- Facial and Body Acne Are Similar
- Physical Irritation of the Skin Can Make Body Acne Worse
- Is Sweat a Cause of Body Acne?
- Severe Forms of Body Acne
- Treating Body Acne
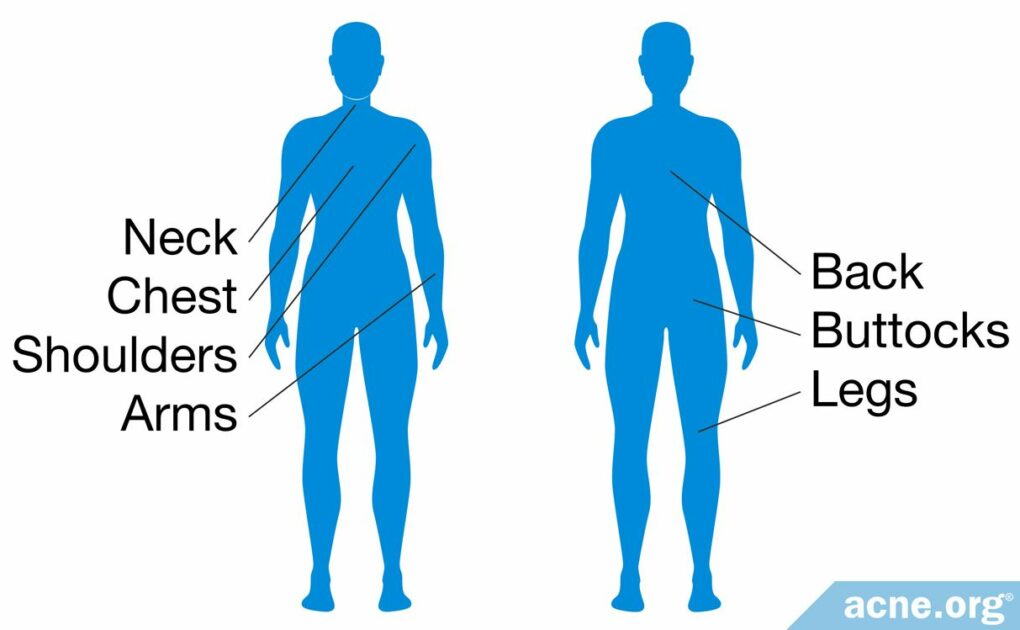
People don’t talk about it much, but acne on the back, chest, and elsewhere on the body is surprisingly common. Areas other than the face where acne can present itself include the:
- Back
- Chest
- Back of the Neck
- Shoulders
- Arms
- Buttocks
- Legs
About One-Half of People with Facial Acne Also Suffer from Body Acne
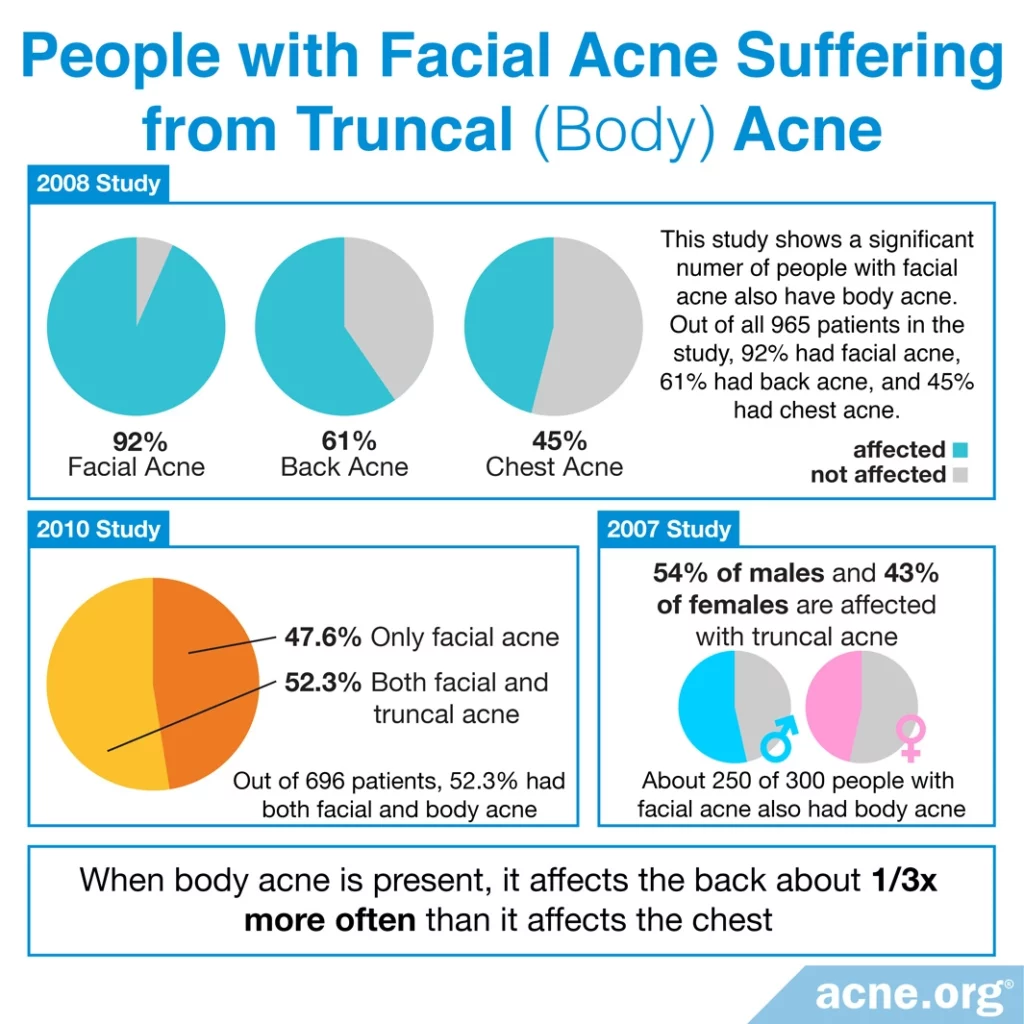
Acne affecting the back and chest is called “truncal acne.” Five studies show us that:
- About half of people who have facial acne also have truncal acne.
- Males tend to experience body acne slightly more often.
- Body acne tends to show up on the back slightly more often than the chest.
Expand to read details of studies

A 2007 study published in the Journal of the American Academy of Dermatology involving 300 patients with facial acne (ages 14 – 30 years) finds that approximately half of the people who have facial acne also have truncal acne. In the group who have truncal acne, the acne is present on the back about one-third times more often than on the chest. The males in this study are affected with truncal acne slightly more often than the females (54% of males and 43% of females).1

Another study, published in 2010 in the Journal of Clinical and Aesthetic Dermatology, including 696 patients from five private practices finds 47.6% have only facial acne, and 52.3% have both facial and truncal acne. Only 2.3% have no facial acne but suffer from body acne.2

The second, more rigorous study was published in the journal Acta Dermato-Venereologica in 2014. In this study, researchers divided 30 patients with mild-A third study, published in 2008 in the Journal of Drugs in Dermatology, including 965 patients with acne finds 92% suffer from facial acne, 45% have chest acne, and 61% have back acne.3

A survey published in the journal Anais Brasileiros de Dermatologia in 2014 finds that out of 2200 Brazilian 18-year-olds, 76% have acne on the face, 31% have acne on the chest, and 50% have acne on the back.4

Finally, a 2015 study published in the Journal of the European Academy of Dermatology and Venereology reports on 374 women with acne from 15 countries around the world. The study finds that 48.4% of women with acne suffer from body acne.5
Body Acne Often Goes Unreported
When acne patients go to see a doctor they often talk only about their facial acne and do not mention their body acne, as we can see from the following 2007 study:

A 2007 study in the Journal of Drugs in Dermatology notes that 1 in 4 patients who have both facial and body acne report only the facial acne. “In patients presenting with a chief complaint of only facial acne, 22.4% also exhibited truncal involvement, which was detected only after clinical inspection of the chest and/or back by the investigator.”
Because acne patients may feel more embarrassment about their facial acne, they sometimes place more importance on getting treatment for the facial lesions. From the same study, “The face was identified by 85% of the patients as the region of involvement which caused them the greatest embarrassment. Other sites identified in descending order were the back (7%), chest (2.5%), and neck (2.2%).”6
Not Enough Research on Body Acne
There is far more research on facial acne compared to body acne. There are many standardized grading systems in place for evaluation of acne, but they are mostly limited to facial acne. Of the 25 grading systems that are available for acne, only 2 of them deal with chest and back acne.7

Similarly, research dealing with the treatment of acne, including topical and systemic medications, also remains focused on facial acne. “While acne is widely recognized to involve the trunk, there is a dearth of information on the prevalence and severity of acne of this region. In part, this may be due to the lack of validated, standardized systems for evaluation of acne for extra-facial regions. Furthermore, investigational studies of acne medications focus on facial acne with scarce attention to other anatomical sites, even for systemic treatments.”6
Facial and Body Acne Are Similar

Body acne develops in a similar way to facial acne, but the pores on the body tend to be larger, so larger acne lesions often develop on the body. However, regardless of location, all acne lesions begin with a clogged pore, which can lead to a backup of skin oil that normally drains out of the pore to the surface of the skin. In this clogged pore, bacteria grows inside the trapped skin oil and acne develops.8,9
Physical Irritation of the Skin Can Make Body Acne Worse
Anything that comes into prolonged contact with the skin can cause acne to become worse. The more the skin is physically irritated, the more chance that acne will develop. This is so well known that it has its own medical term: acne mechanica.

Authors in the Canadian Medical Association Journal describe acne mechanica that they find on the body in this way: “It usually occurs in areas covered by protective gear in contact sports. For instance, football players often have (acne) on the… shoulders… Golfers can experience acne mechanica on the lateral back where the strap of their golf bag rubs.10
Acne mechanica affects athletes but can also affect people who, for instance, wear heavy backpacks throughout the day. However, obviously, it is impossible to avoid contact with the body throughout the day. Rather than attempting to eliminate all physical irritation of the body, simply become aware of major and obvious sources of irritation to the body and eliminate them when possible. Then, treat the body with a proper anti-acne body regimen and you can stay clear. A quick note: Sports gear can also cause allergic dermatitis, a condition which is often mistaken for acne mechanica. It results from substances in the gear itself and can look like acne:

“Allergic contact dermatitis caused by substances found in sports equipment (e.g., rubber chemicals such as thiurams, mercaptobenzothiazole and carbamates) needs to be considered in the differential diagnosis of acne mechanica.”10 Doctors use patch testing to tell the difference between acne mechanica and allergic dermatitis.

Is Sweat a Cause of Body Acne?
People have often wondered whether exercise-induced sweat is a cause of body acne or not. Sweat itself is not a problem since there is nothing in sweat that would cause acne, but sweat, when combined with physical irritation, might make the irritation worse. We only have one study that looks at this directly and that study was too small to draw a conclusion, but it is hypothesized that sweat + physical irritation might lead to more clogged pores than physical irritation on its own.
A 2008 study published in Pediatric Dermatology took a look at this question. The study required young, active males to exercise long enough to induce sweating. The study took place over five days per week during a two-week period and included three separate groups:
- Group 1 was the control group for comparison that did not exercise
- Group 2 showered after one hour of exercise
- Group 3 showered after four hours of exercise
Although results showed there were more acne lesions in groups that exercised, due to the small sample size and wide differences in number of lesions, the results could not reach statistical significance. It was concluded the role of exercise-induced sweat in body acne has to be confirmed through a more rigorous, larger sample study.11
Severe Forms of Body Acne
Body acne is often present along with facial acne and is usually not related with any other diseases or conditions. There are, however, two rare conditions which can affect both the face and the body:
- Acne conglobata is a very uncommon, extremely severe form of acne. It affects the chest, back, buttocks, and face. It is very challenging to treat and can result in disfiguring scars, which is the cause of immense anxiety and stress in patients.12
- Acne fulminans is the only other rare condition that presents with body acne. This type of acne usually occurs between the ages of 13 – 16 years, primarily in Caucasian males, and is characterized by severe acne lesions on the face, upper chest, and back. Other symptoms include fever, chills, body pain, and weakness. In a few cases acne fulminans may affect the bones, muscles, liver, and spleen.13
Treating Body Acne
The same treatments that work for facial acne can also successfully treat body acne. For mild-to-moderate body acne, a regimen consisting of topical benzoyl peroxide and glycolic acid is most effective. For severe, deeply scarring body acne, isotretinoin (Accutane®) may be an option. A variety of other treatments are also available.14-17
Eating a low-carb, keto style diet may also surprise you. Eating this way should theoretically reduce inflammation and regulate hormones, and might help get your body acne under control. It’s worth a shot because it’s also a very healthy way to eat. Just make sure you keep lots of veggies in your diet to ensure you have all the antioxidants your skin needs.
References
- Del Rosso, J. Q., Bikowski, J. & Baum, E. Prevalence of truncal acne vulgaris: A population study based on private practice experience. J. Am. Acad. Dermatol. 56, AB3 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17668525
- Bikowski, J. A review of the safety and efficacy of benzoyl peroxide (5.3%) emollient foam in the management of truncal acne vulgaris. J. Clin. Aesthet. Dermatol. 3, 26 – 29 (2010). https://www.ncbi.nlm.nih.gov/pubmed/21103313
- Tan, J. K. et al. Prevalence and severity of facial and truncal acne in a referral cohort. J. Drugs. Dermatol. 7, 551 – 556 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18561586
- Isaacsson, V. C., Almeida, H. L. Jr, Duquia, R. P., Breunig, J. de A. & Souza, P. R. Dissatisfaction and acne vulgaris in male adolescents and associated factors. An. Bras. Dermatol. 89, 576-579 (2014). https://pubmed.ncbi.nlm.nih.gov/25054743/
- Dréno, B., Thiboutot, D., Layton, A. M. et al. Large-scale international study enhances understanding of an emerging acne population: adult females. J. Eur. Acad. Dermatol. Venereol. 29, 1096-1106 (2015). https://pubmed.ncbi.nlm.nih.gov/25296739/
- Del Rosso, J. Q. et al. A closer look at truncal acne vulgaris: prevalence, severity, and clinical significance. J. Drugs Dermatol. 6, 597 – 600 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17668525
- Tan, J. K., Zhang, X., Jones, E. & Bulger, L. Correlation of photographic images from the Leeds revised acne grading system with a six-category global acne severity scale. J. Eur. Acad. Dermatol. Venereol. 27, e414 – 419 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22924863
- Handa, S. Propionibacterium Infections (2015) https://emedicine.medscape.com/article/226337-overview
- Mourelatos, K., Eady, E. A., Cunliffe, W. J., Clark, S. M. & Cove, J. H. Temporal changes in sebum excretion and propionibacterial colonization in preadolescent children with and without acne. Br. J. Dermatol. 156, 22 – 31 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17199562
- Freiman, A., Barankin, B. & Elpern, D. J. Sports dermatology part 1: common dermatoses. CMAJ 171, 851 – 853 (2004). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC522647/
- Short, R. W., Agredano, Y. Z., Choi, J. M. & Kimball, A. B. A single-blinded, randomized pilot study to evaluate the effect of exercise-induced sweat on truncal acne. Pediatr. Dermatol. 25, 126 – 128 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18304176
- Shirakawa, M., Uramoto, K. & Harada, F. A. Treatment of acne conglobata with infliximab. J. Am. Acad. Dermatol. 55, 344 – 346 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16844527
- Zaba, R., Schwartz, R., Jarmuda, S., Czarnecka-Operacz, M. & Silny, W. Acne fulminans: explosive systemic form of acne. J. Eur. Acad. Dermatol. Venereol. 25, 501 – 507 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21029206
- St Surin-Lord, S. & Miller, J. Topical treatment of truncal acne with tretinoin lotion 0.05% and azelaic acid foam. Case Rep. Dermatol. Med. 2020, 5217567 (2020). https://pubmed.ncbi.nlm.nih.gov/32257457/
- Del Rosso, J. Q., Kircik, L. & Tanghetti, E. Management of truncal acne vulgaris with topical dapsone 7.5% gel. J. Clin. Aesthet. Dermatol. 11, 45-50 (2018). https://pubmed.ncbi.nlm.nih.gov/30214667/
- Blume-Peytavi, U,, Fowler, J., Kemény, L., et al. Long-term safety and efficacy of trifarotene 50 μg/g cream, a first-in-class RAR-γ selective topical retinoid, in patients with moderate facial and truncal acne. J. Eur. Acad. Dermatol. Venereol. 34, 166-173 (2020). https://pubmed.ncbi.nlm.nih.gov/31306527/
- Tan, J., Thiboutot, D., Popp, G. et al. Randomized phase 3 evaluation of trifarotene 50 μg/g cream treatment of moderate facial and truncal acne. J. Am. Acad. Dermatol. 80, 1691-1699 (2019). https://pubmed.ncbi.nlm.nih.gov/30802558/